This is important because, if the patient is accurate, then the sceptical physician may under-treat and risk future disability. If the patient is catastrophising, then an algorithm-driven treatment plan may result in risky therapeutic escalation.
Associations of catastrophising are:
1) seronegativity
2) lack of objective damage (joint erosions)
3) fibromyalgic phenotype (neuropathic pain and central sensitization).
Global disease activity measures increasingly (and rightly) incorporate patient reported outcomes (pain, fatigue, function, quality of life) to more objective clinical measures (tender/swollen joints, ESR/CRP). Art and Science.
A somatization comorbidity phenotype impacts response to therapy in rheumatoid arthritis: post-hoc results from the certolizumab pegol phase 4 PREDICT trial
arthritis-research.biomedcentral.com
Patients who catastrophise will skew disease activity measures heavy on patient reported outcomes to show poor response to any therapeutic agent.
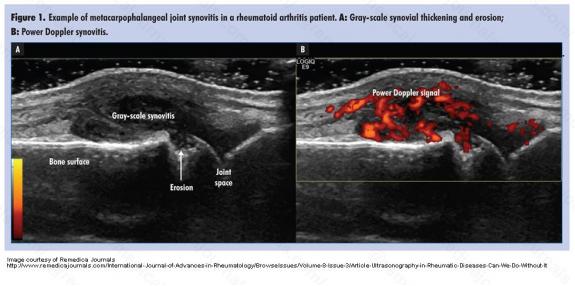
Ultrasound of the hand is sufficient to detect subclinical inflammation in rheumatoid arthritis remission: a post hoc longitudinal study
The answer lies in what one chooses as the ultimate target/goal of treatment: prevention of significant radiographic progression (joint damage) likely to cause permanent disability, or patient-centred outcomes encompassing pain, fatigue, strength, function and quality of life.
If one chooses the first, then PDUS-guided treat-to-sonographic-remission-target may be an overkill. But if one aims for the latter, then the evidence suggests that even the stringent EULAR Boolean remission criteria may fall short.
clinexprheumatol.org
Ultrasound of the Extensor Carpi Ulnaris and Tibialis Posterior tendons for tenosynovitis, if present before commencement of biologic treatment, can be useful to gauge treatment response.
Changes in clinical disease activity are weakly linked to changes in MRI inflammation on treat-to-target escalation of therapy in rheumatoid arthritis

While MRI inflammation measurement corresponds to the clinical measure called DAS-CRP, it does not appear to be sensitive to the clinical change/improvement indicative of clinical remission.
It’s plausible that, as in PDUS, many patients in clinical remission continue to have radiological evidence of active disease. The question is whether this degree of disease activity would translate to significant future damage, disability or impaired quality of life, which would therefore warrant therapeutic intensification. At this point, we don’t know.



