
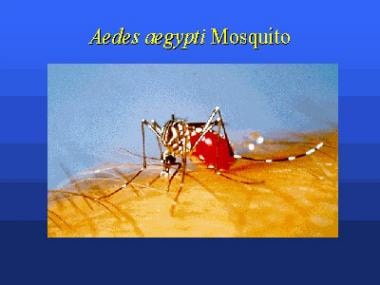
Zika, Chikungunya and Dengue. These viruses share the same vector: the Aedes aegypti mosquito. Arthralgia, or outright arthritis, can be the predominant presenting symptom.
How to Spot Chikungunya and Its Mimics

The potentially life-threatening aspects of Dengue infection, namely Dengue Haemorrhagic Fever and Dengue Shock Syndrome, are immune-mediated.
90% of these occur in the context of a secondary Dengue infection with a different serotype. A prominent immune mechanism accounting for this phenomenon is Antibody Dependent Enhancement (ADE).
The antibodies produced are specific against the previously encountered/vaccinated serotype, but they can cross-react with the current (and different) serotype without neutralising it. Instead, these antibodies facilitate viral uptake into monocytes and macrophages through Fc-receptor binding, thereby acting like trojan horses. Once inside the target cells, viral replication runs amok, triggering a massive Th1 and Th17 immune response, eventually culminating in a cytokine storm.
If such an immunological mechanism is accurate, there are 2 important implications:
1) immunomodulation with targeted therapies like anti-TNF and anti-IL17A may emerge as feasible adjuncts in the treatment of severe Dengue complications, beyond the current merely supportive paradigm;
2) vaccinations which do not cover all 4 serotypes may do more harm than good by priming an entire previously unexposed populace for ADE.
Dengue virus sero-cross-reactivity drives antibody-dependent enhancement of infection with zika virus

“Plasma immune to DENV showed substantial cross-reaction to ZIKV and was able to drive antibody-dependent enhancement (ADE) of ZIKV infection.”
This is worrisome if true. Is ADE the pathogenic mechanism for the autoimmune phenomena like Guillain-Barre Syndrome, and perhaps even microcephaly? The Dengue-endemic populace would therefore naturally be at far higher risk to develop such complications from Zika infection.


